
Preventing delirium in the hospital
By: Alexandra Curkovic, clinical nurse specialist, Hospital Elder Life Program
Have you ever heard of delirium? This disorder isn’t commonly understood, but it is a common concern among older adults in the hospital (it can also affect kids).
It’s an acute disorder, which means it usually appears suddenly and doesn’t typically last too long. It can develop in as little as a few hours and symptoms tend to fluctuate in severity throughout the day. People with delirium have problems in attention and awareness. It is most common in older patients who are hospitalized, but the symptoms are not always easy to identify.
A patient with delirium may have difficulty following a conversation and may get confused about their environment to the point that they don’t recognize they are in the hospital. Changes to the patient’s physical environment—like moving a patient to a new room—may make symptoms worse.
What does hospital delirium look like?
People with delirium can act confused and may:
• have trouble paying attention
• be forgetful
• be restless and upset
• have trouble concentrating
• startle easily to any sound or touch
• slur their speech
• ramble and jump from topic to topic
• not know where they are
• have trouble staying awake
• see and hear imaginary things
• mix up days and nights
• act confused for a short period of time during the day and then be suddenly okay
• drift into sleep during conversation
Delirium can have serious, negative effects on a person’s ability to function independently and can affect their quality of life long term. It can also increase a person’s likelihood of developing dementia.
A patient’s perspective on delirium
John Vlainic, a former Hamilton Health Sciences employee, experienced delirium while he was in the hospital being treated for a serious infection. He describes the experience as completely disorienting.
“I remember being adamant there were men on the roof”
“I remember being adamant there were men on the roof outside my hospital room window,” he says, recalling one of the visions he imagined. “I also became convinced the machine warming my oxygen was dangerous. I decided I would unplug it in the middle of the night.”
John’s wife Ruth says it was concerning seeing her husband in this state. They were glad when his delirium started to lift after a couple days.
What’s the difference between dementia and delirium?
Dementia develops over months, with a slow progression of cognitive decline over years. On the other hand, delirium occurs abruptly over a few days or weeks, and symptoms can come and go during the day. A person with dementia is much more likely to develop delirium when hospitalized.
The main difference separating delirium from dementia is inattention and level of alertness. The individual with delirium simply cannot focus on one idea or task. This inattention is usually present in later stages of dementia.
Level of consciousness for patients with delirium may fluctuate from very tired to very easily startled state whereas patients with dementia are normally alert unless they are in the later stage.

Risk factors for hospital delirium
There are several risk factors that can make a person more likely to develop delirium. The tips below will help you to reduce these risk factors in the hospital:
1. Cognitive impairment: People with existing dementia or mild cognitive impairment are more likely to develop delirium. Look out for signs of changes in thinking like memory loss or difficulty with daily tasks.
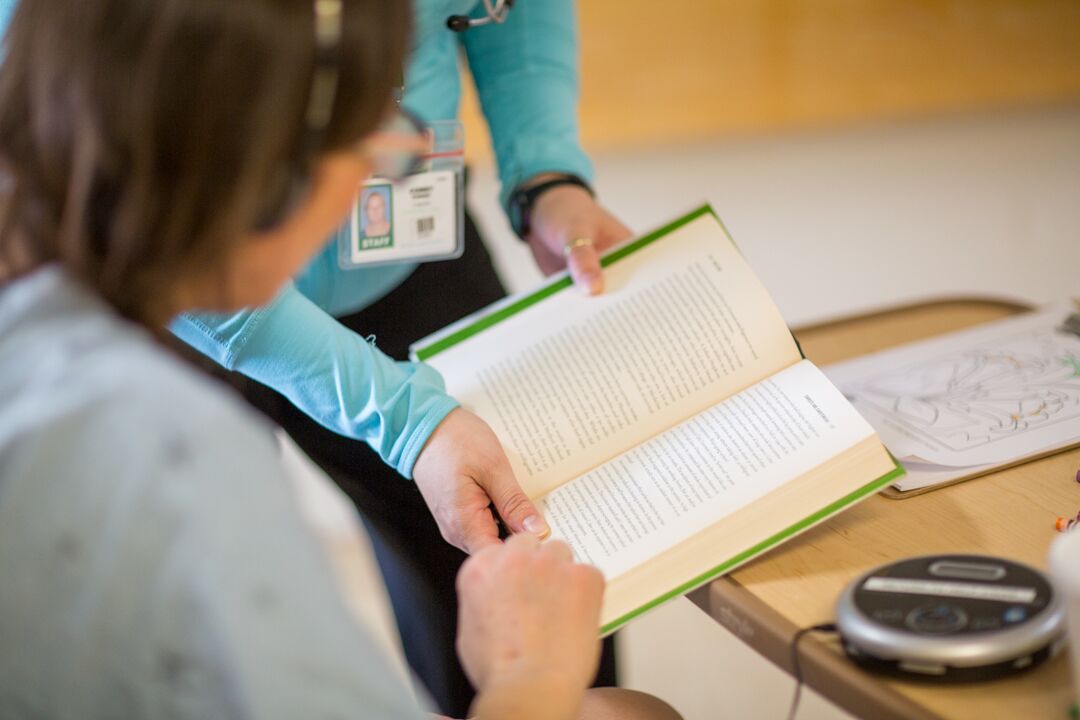
How to help: If someone has cognitive impairment, keep their mind active while they’re in the hospital. Ask questions about current season, holidays, past hobbies and family members. Bring familiar items, like board games or books to their room to help occupy them.
2. Sensory impairment: Hearing or vision loss can make it more difficult for someone to assess their surroundings and can contribute to delirium.
How to help: Bring their sensory aids with you to the hospital and label them. If they typically wear hearing aids or glasses, make sure they wear them during their hospital stay.
3. Loss of mobility: Lack of movement can make someone more likely to develop delirium. A patient who walked independently before hospitalization may feel unsteady during their illness or after an operation, and need assistance with a walker or other mobility device.
How to help: Advocate for removal of tethers such as IVs and oxygen tubes, and urinary catheters. Encourage the patient to move throughout the day to keep their muscles strong. Family members can help!
4. Dehydration: When people get dehydrated, they are significantly more likely to develop delirium.
How to help: Watch out for physical indicators of dehydration like muscle weakness, speech difficulty, dry mouth and a pale lining inside of the mouth. Encourage drinking throughout the day. Talk to the care team to make sure your loved can safely drink.
5. Recently added medications: New medications can increase someone’s risk of delirium. The medications most often associated with delirium are benzodiazepines and anticholinergics.
How to help: Discuss alternative medications with the care team to reduce risk.

If delirium develops while your loved one is in hospital
• Tell the staff right away if you see a change in thinking.
• Develop a plan of care with the staff to help with the confusion.
• Try to redirect to current season, date and place. Explain why they are in the hospital. You may need to repeat this many times. Do not argue if they see things differently.
• Continue to ensure glasses and hearing aids are worn if needed.
• Continue to ensure your loved one is eating and drinking well. Ask your nurse if it is okay to feed your love one.
• Continue to encourage walking.
Hamilton Health Sciences has a Hospital Elder Life Program (HELP) service available for patients over 75 who are in select clinical areas at Hamilton General Hospital or Juravinski Hospital. If your loved one develops delirium, ask if these services are available on their unit. Click here for more information about the HELP Program.
