“I changed my goal from saving his life to saving his childhood.”
Ten-year-old Meric has a rare life-limiting disease that requires frequent monitoring and care by a team of health care providers, but he hasn’t stayed overnight in a hospital for more than a year — and that’s exactly what his family wants.
Meric was born a happy, healthy boy who showed no signs of the challenges ahead. That changed when he was three years old and had his first seizure. He became unstable on his feet and began to lose his speech and vision.
After many doctor’s appointments and rounds of genetic testing at the Neuromuscular and Neurometabolic Clinic at Hamilton Health Sciences’ McMaster Children’s Hospital (MCH), Meric was diagnosed with Batten’s disease, a neurodegenerative disease that affects his brain and spinal cord. Batten’s disease is a progressive disease, which means it worsens over time. Sadly, Meric is expected to die while still a child.
Meric was quickly referred to MCH’s pediatric palliative care program, the Quality of Life and Advanced Care program (QoLA Care, pronounced like “koala,” for short), which was scary for his family.
“it’s not end-of-life care, but the focus is on quality of life for the entire journey”
“I knew the diagnosis and the prognosis, but I always associated palliative care as the end stages,” says Lisa, Meric’s mother. “It wasn’t until we met with them and they explained their role that I started to understand that it’s not end-of-life care, but the focus is on quality of life for the entire journey. Working with QoLA didn’t signify the end of our journey, but taking them on made our journey smoother and so much more comforting. That kind of support is amazing.”
For some families, receiving care in the comfort of their home instead of regularly visiting the hospital is one of their goals in order to enhance a patient’s quality of life. This goal is fully supported by the QoLA Care team, who have processes and resources in place to deliver seamless palliative care from hospital to home.
What is palliative care?
The goal of palliative care is to enhance the quality of life for people with life-limiting conditions and their families. Palliative care can be provided from early in the illness through to bereavement, and extends beyond physical care to include emotional, social, and spiritual support that aligns with a family’s goals.
In the QoLA Care program, support can start at birth, or even before, and continues through young adulthood. The program works to limit sources of suffering and increase opportunities for joy and precious moments for pediatric patients, their families, and their loved ones.
Palliative care for improved quality of life
Once his family learned Meric’s disease had no cure, they shifted their focus from, “how are we going to fix the problem?” to “how are we going to make his time the best it can be?”
Meric would visit the hospital for acute conditions – something that was new and severe — such as pneumonia or an infection at the site of his feeding tube. But for difficult symptoms related to his underlying condition, or for times they faced challenging decisions for their son, Lisa could call or text a member of the QoLA Care team to help. The team would provide virtual care or come directly to their home to support the family.

Meric’s mom Lisa says she will never forget the support and compassion her family received from QoLA Care.
“We live in Milton and MCH is in Hamilton, so having that person to contact versus having to run to emergency every other week with a question helped us avoid bringing my medically complex child to an area where other children were sick with colds and flus,” says Lisa. “Now that we’re nearing the end of our journey, QoLA Care is going to be even more instrumental in helping us stay where we want to be,” – and that is in their home.
“Now that we’re nearing the end of our journey, QoLA Care is going to be even more instrumental in helping us stay where we want to be.”
QoLA Care helped shift the focus from changing the outcome of Meric’s disease to managing symptoms to improve his quality of life. “I changed my goal from saving his life to saving his childhood,” says Lisa. “We knew we had control over how his days were going to be spent and how we were going to keep him comfortable and happy in the days we have left with him.”
More in-home support
A historic recent investment from the provincial government has allowed QoLA Care to operate as the region’s specialized pediatric palliative care program. The program now includes doctors, clinical specialists, a perinatal outreach nurse practitioner, a child life specialist, a social worker, a system navigator, and a community outreach nurse practitioner.
Brittany Gold is a new system navigator who acts as a liaison between MCH and community partners. She is responsible for organizing the flow of care, including appointments, meetings with home care, mental health supports, schools and other key providers needed to ensure a family’s support network is working in partnership with one another and in alignment with their goals.
“Kids are amazing. They are incredible, resilient, strong, brave.”
As the new palliative care social worker, Bethany Sprowl supports families throughout their journey by counselling patients and family members, facilitating peer support groups, and assisting with social and financial issues.
There will soon be an additional clinical specialist joining QoLA Care’s perinatal program to support parents whose baby may not survive birth, or who may be born with serious, life-threatening complications.
The program has also added a community outreach nurse practitioner, Emily Skoutarou. Often, the expertise needed to care for serious and rare conditions like Meric’s is found within specialty children’s hospitals. Skoutarou extends palliative care expertise from the children’s hospital into children’s homes.

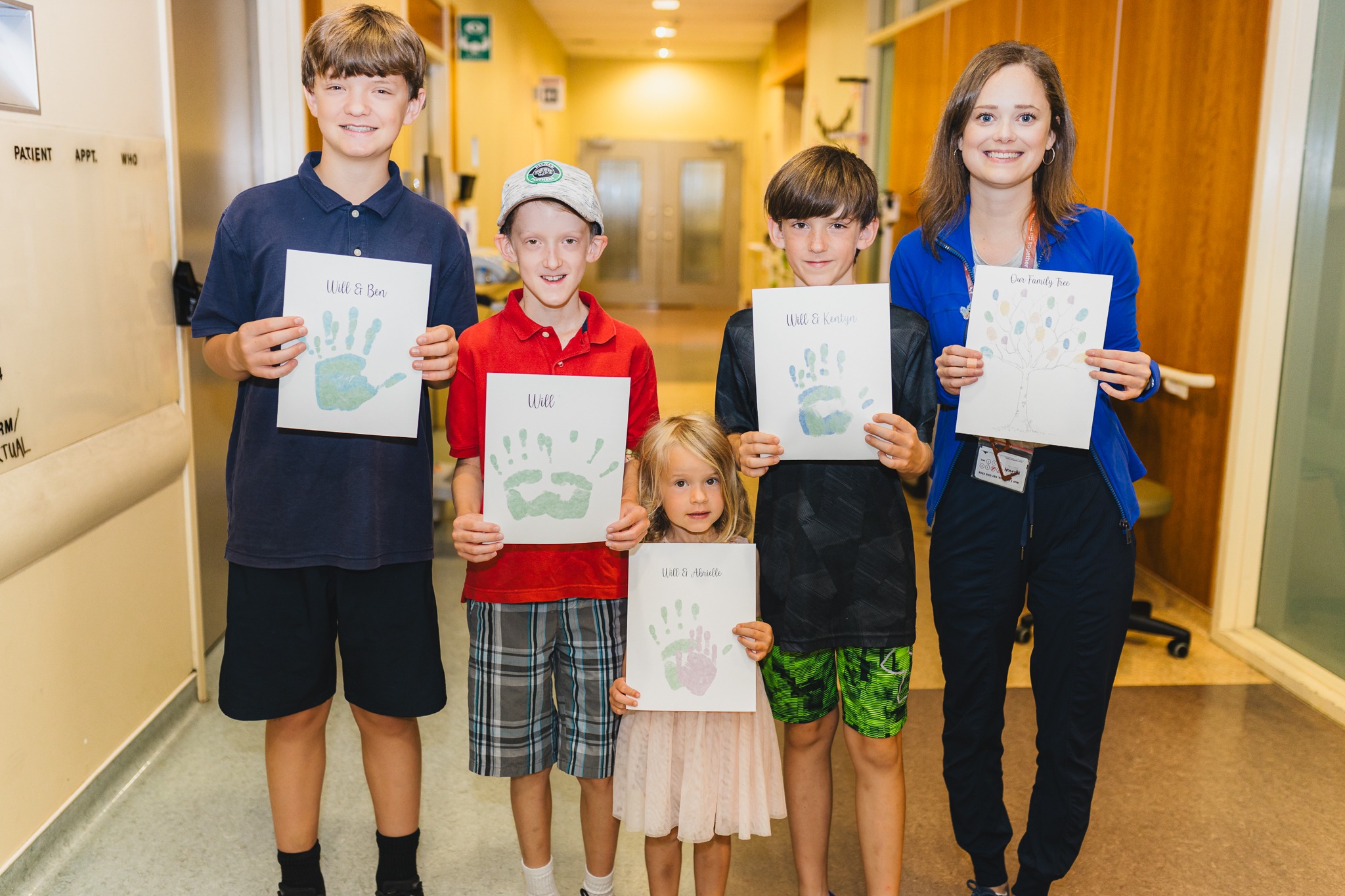
Meric surrounded by just some of his support team: his mom Lisa, nurse practitioner Emily Skoutarou and clinical specialist Cindy Van Halderan.
New nurse practitioner and in-home pediatric palliative care specialist
Skoutarou joined QoLA Care just months ago and has been working closely with Meric and his family through home visits and phone calls. She has worked at HHS before, but has also worked as a pediatric palliative care nurse for over ten years at a children’s hospice in Toronto.
Her role is to support children with palliative needs, and their families, while they are at home – especially near the end of life. She follows up with home visits routinely or as needed to assess a child in their own bed and diagnose and treat any symptoms they may be experiencing. If a new need arises, Skoutarou and her QoLA Care colleagues develop a new care plan which may involve medication or other physical, emotional, or spiritual support, and guide caregivers to manage any challenges that may arise.

Nurse practitioner Emily Skoutarou says children are the real superheroes.
“If children are going home, whether that’s for symptom support or for end-of-life care at home, I would see them in the hospital and help bridge that gap at home to make sure those supports are in place,” says Skoutarou. “For example, making sure they have the equipment that can support their care, that their in-home nursing support is feeling comfortable with new care plans, and that families have a step-by-step symptom management plan if a symptom escalates at home.”
Skoutarou also supports other nurses in the community provided by Ontario’s Home and Community Care Support Services to ensure they are equipped to care for these patients, and stays in contact with the care coordinator to manage the nursing needs in the community. For many community nurses, providing palliative care to children at home is new, so having expert guidance is key to delivering the best care to children in need.
Recently, she facilitated a virtual education session with community nurses to ensure the full team understands what to anticipate with Meric’s disease progression and how to manage his symptoms. This knowledge sharing creates a strong and supportive network across Meric’s health care partners.
Families can call her directly as needed during working hours, or they can call an on-call QoLA Care doctor 24/7 for emergencies.
Support, compassion, and meaningful moments
Meric uses a wheelchair, feeding tube, and is supported by in-home oxygen and suction. He isn’t able to speak. But with the support of his home nursing team, his health care team at MCH including Neurology, Complex Care and QoLA Care, and his school supports, Meric is able to receive support for his physical needs while still enjoying elements of a childhood that are meaningful to him and his family.
“QoLA Care have kept us in our home where we wanted to be. They really helped us maximize our time with Meric, because it is limited.”
The last couple of weeks have been difficult for Meric and his family, but Skoutarou and the QoLA Care team have supported them along the way. “QoLA Care have kept us in our home where we wanted to be. They really helped us maximize our time with Meric, because it is limited,” says Lisa. “I will never forget the support and compassion they’ve provided the entire journey. I’m sure they will be incredible at the end stages as well, but what will always stand out is the years of support.”
To Skoutarou, it’s the children who are the real heroes.
“There are children who have life-limiting illnesses that need our support. As health care professionals, our job is not just to preserve their life, but to focus on quality of life,” she says. “Kids are amazing. They are incredible, resilient, strong, brave. They are the ones who are persevering through some very hard things, along with their families. It is my privilege to be part of their journey. They are the superheroes.”
Expanding support with new pediatric hospice
On May 23, 2024, the QoLA Care team at MCH joined their partners Kemp Care Network to announce the construction of a new children’s hospice in Dundas, Ontario – Keaton’s House – Paul Paletta’s Children’s Hospice. It will be located just minutes down the road from McMaster Children’s Hospital and is expected to open in 2026.
Supported by the Ministry of Health, the City of Hamilton, and a number of partners across the region, this will be a home-like setting with hospital-grade equipment and medications, where young people with life-limiting conditions can be cared for by MCH’s palliative care experts.
This hospice will help advance the regional pediatric palliative care program that cares for families in the hospital, at home, or in the new hospice. The hospice will fill a critical missing component of pediatric care in the Hamilton Region.